On This Page
The landscape of modern medicine is currently undergoing a radical transformation as researchers move away from traditional prosthetic replacements and toward the biological activation of the body's own healing mechanisms. In situ tissue regeneration represents the pinnacle of this shift, offering a future where damaged organs and complex tissues can be fully restored to their original functional state without the need for external stem cell injections or invasive donor transplants.
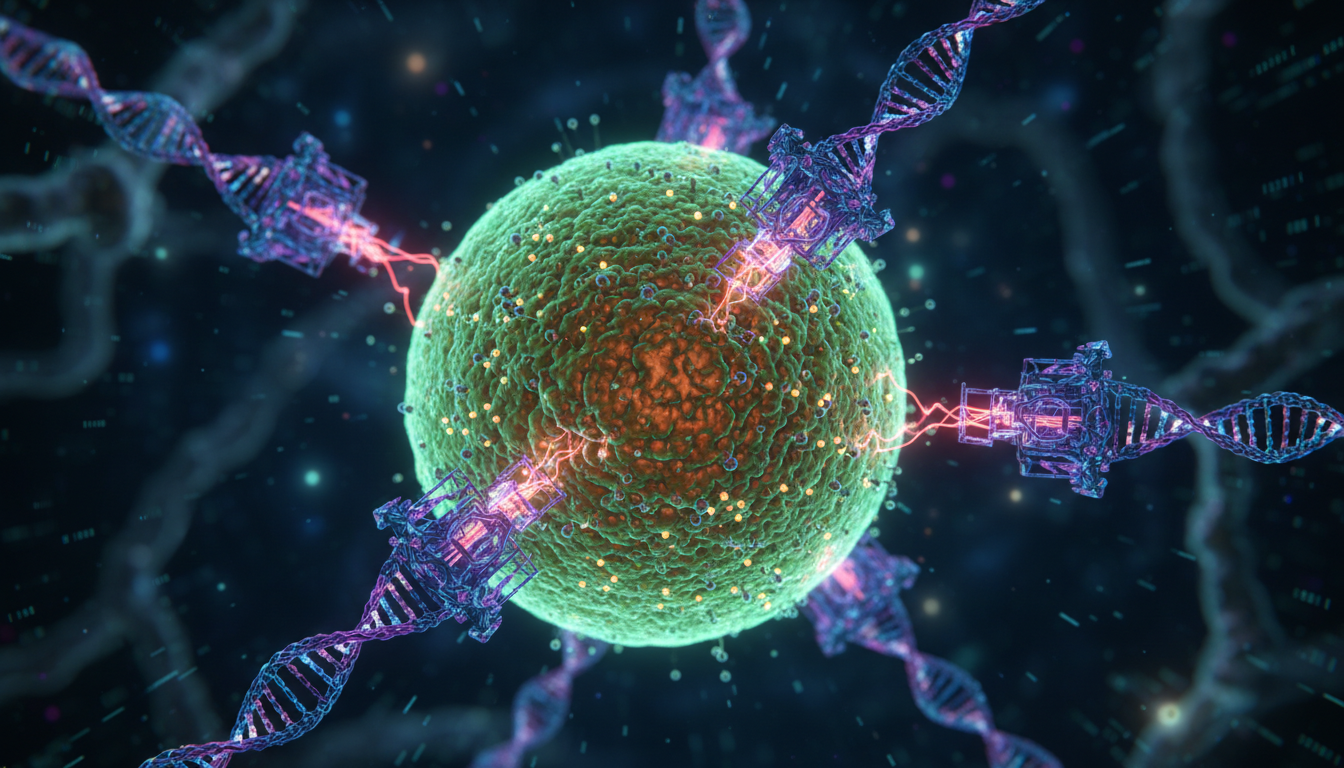
Recent discoveries in 2026 have highlighted the existence of latent genetic instructions within the human genome that closely mirror the regenerative powers seen in amphibians like the axolotl. By understanding how to manipulate these "salamander genes," scientists are unlocking the ability to inhibit the natural scarring response and instead promote the growth of functional bone, nerve, and skin tissue directly at the site of the injury.
We Also Published
The Biological Foundation of In Situ Tissue Regeneration
To understand how in situ tissue regeneration functions at a molecular level, we must first examine the evolutionary history of wound healing and the divergent paths taken by different species. While mammals typically prioritize rapid wound closure through fibrosis and scarring, other vertebrates have retained the ability to undergo epimorphic regeneration, allowing for the complete replacement of lost appendages and complex internal organs.
The primary challenge for human regenerative biology has been identifying why our cells possess the genetic toolkit for regeneration but fail to utilize it effectively following a traumatic injury. By mapping the regulatory networks that control cell plasticity, researchers are now identifying the specific chemical signals required to revert mature human cells into a progenitor-like state that can facilitate the organized growth of new biological structures.
Lessons from the Axolotl and Salamander Models
The axolotl has long served as the gold standard for studies in in situ tissue regeneration due to its incredible ability to regrow limbs, spinal cords, and even portions of its brain. Unlike humans, these creatures do not form scar tissue; instead, they form a specialized structure known as a blastema, which is a mass of undifferentiated cells capable of growth.
Research into the axolotl genome has revealed that their regenerative success is tied to specific gene clusters that remain active throughout their entire lives, whereas humans typically deactivate these pathways after embryonic development. By isolating these genetic sequences, biologists have identified the fundamental blueprints required to orchestrate the complex spatial arrangement of different cell types during the limb regrowth process.
One of the most critical aspects of salamander regeneration is the management of the immune system, which works in tandem with local cells to prevent the accumulation of collagen. In these amphibians, macrophages play a vital role in clearing debris and secreting growth factors that encourage cell division rather than the dense, restrictive fiber networks that characterize human wound healing.
Furthermore, the nervous system of the salamander provides essential neurotrophic factors that signal the blastema to continue expanding until the missing part is fully replaced. This intricate communication between the nerves and the surrounding tissue ensures that the regenerated limb is perfectly proportional and functional, a feat that researchers are now attempting to replicate in human clinical trials.
By studying the specific proteins secreted by axolotl cells, scientists have begun to develop synthetic analogs that can be applied to human wounds to mimic this regenerative environment. These efforts are the cornerstone of in situ tissue regeneration, as they provide the necessary biochemical cues to convince human cells that they are still in a developmental, rather than a healing, phase.
Decoding the Human Dormant Regenerative Genome
The human genome contains a vast array of "evolutionary echoes" or dormant genes that were once active in our distant ancestors but have since been silenced by epigenetic mechanisms. In situ tissue regeneration seeks to identify these specific sequences and determine the exact molecular switches required to turn them back on during times of critical physical need or tissue loss.
Recent advances in CRISPR technology and epigenetic profiling have allowed scientists to see that many of the genes responsible for limb development in the womb are still present in adult cells. These genes are often wrapped tightly in chromatin, making them inaccessible to the cell's transcriptional machinery, which prevents the body from naturally initiating a regenerative response after a major injury.
The goal of modern restorative medicine is to use small molecules to modify the epigenetic landscape, effectively "unwrapping" these dormant genes so they can be expressed at the site of trauma. This process does not involve changing the DNA sequence itself but rather changing how the cell reads its own internal instructions to prioritize growth over scar formation.
By comparing the transcriptomes of regenerating salamanders with those of healing humans, researchers have found a surprising amount of overlap in the basic genetic machinery. The difference lies primarily in the timing and duration of gene expression, suggesting that the human body has the hardware for regeneration but lacks the updated software to run the process correctly.
As we continue to decode these dormant pathways, the possibility of in situ tissue regeneration becomes more tangible, moving from the realm of science fiction into practical medical application. Understanding these genetic "switches" is essential for developing therapies that can safely and effectively awaken the regenerative potential buried deep within our own biological makeup for better health.
Molecular Mechanisms and the Hippo Signaling Pathway
At the heart of the cellular decision-making process for in situ tissue regeneration is a complex network of proteins known as the Hippo signaling pathway. This pathway acts as a critical regulator of organ size, cellular proliferation, and apoptosis, ensuring that tissues grow to the correct dimensions and stop once their functional goals are achieved.
In the context of regeneration, the Hippo pathway functions as a sensory mechanism that detects changes in cell density and mechanical tension within the tissue environment. When an injury occurs, the pathway must be precisely modulated to allow for a burst of cellular division while preventing the uncontrolled growth that could lead to the formation of tumors or other malignancies.
Regulating Organ Size and Cellular Proliferation
The Hippo signaling pathway consists of a kinase cascade that ultimately controls the activity of two key transcriptional co-activators known as YAP and TAZ. When the Hippo pathway is "on," it inhibits YAP and TAZ, preventing them from entering the nucleus and driving the expression of genes associated with cell growth and survival.
For in situ tissue regeneration to occur, the Hippo pathway must be temporarily suppressed, allowing YAP and TAZ to accumulate in the nucleus and initiate a program of rapid cell multiplication. This temporary "release of the brakes" is what enables the body to generate the vast number of new cells required to replace a missing or damaged organ part.
Researchers have found that by manipulating the mechanical environment of a wound, they can influence Hippo signaling to favor regeneration over scarring. Cells sense the stiffness of their surroundings through integrins, and a softer, more embryonic-like matrix can signal the Hippo pathway to remain inactive, thereby promoting the continued proliferation of healthy, functional tissue cells.
In various animal models, the activation of YAP has been shown to trigger the regeneration of heart tissue and liver mass, even in species that typically have limited healing capacity. This suggests that the Hippo pathway is a universal regulator of regenerative potential across the animal kingdom, making it a primary target for new pharmacological interventions and therapies.
However, the precision of this regulation is paramount, as the prolonged activation of YAP/TAZ is a known driver of various types of cancer. Therefore, the future of in situ tissue regeneration depends on our ability to develop "smart" drugs that can transiently inhibit the Hippo pathway only at the site of injury and only for a specific duration.
Overcoming the Scarring Response and Fibrosis
One of the greatest obstacles to in situ tissue regeneration in humans is the body's natural tendency to form scar tissue, a process known as fibrosis. While scarring is an effective way to quickly seal a wound and prevent infection, the resulting dense collagen matrix creates a physical barrier that prevents new cells from migrating.
Fibrosis is driven by specialized cells called myofibroblasts, which are activated by inflammatory signals and begin secreting large amounts of extracellular matrix proteins. To achieve true regeneration, we must find ways to inhibit the activation of these myofibroblasts or encourage them to revert into a more quiescent, non-scarring state during the healing process.
Recent studies have shown that by using small molecule inhibitors to block the TGF-beta signaling pathway, researchers can significantly reduce the amount of scar tissue formed after an injury. This creates a "permissive environment" where the body's natural regenerative signals can take over, allowing for the growth of functional tissue rather than a non-functional fibrous plug.
The relationship between the inflammatory response and in situ tissue regeneration is also being closely examined, as certain types of immune cells are known to promote healing while others promote scarring. By modulating the local immune environment, it is possible to recruit "pro-regenerative" macrophages that assist in the remodeling of the tissue and the support of new growth.
Ultimately, overcoming fibrosis is about changing the body's priority from "survival at any cost" to "functional restoration." By slowing down the initial wound closure and preventing the rapid deposition of collagen, we can give the body the time it needs to activate its dormant regenerative genes and rebuild the damaged structures correctly.
The Rise of Regenerative Pharmacopoeia
The transition toward in situ tissue regeneration is being fueled by a new class of medical treatments known as "Regenerative Pharmacopoeia." These are not traditional drugs that simply treat symptoms, but rather complex biochemical tools designed to provide specific instructions to the body's cells, guiding them through the intricate process of rebuilding lost tissue.
This approach focuses on the use of small molecules, growth factors, and gene-silencing RNAs that can be delivered directly to the site of an injury. By creating a localized "healing cocktail," clinicians can jumpstart the regenerative process without the systemic side effects often associated with traditional pharmaceutical interventions or the complexities of cell-based therapies.
Small Molecules and Chemical Induction Strategies
Small molecules are particularly attractive for in situ tissue regeneration because they are stable, easy to manufacture, and can penetrate deep into tissues to reach the target cells. These chemicals are designed to interact with specific receptors or enzymes that control cell identity, allowing researchers to "reprogram" cells in their natural environment.
Chemical induction strategies involve using a sequence of different molecules to guide cells through the various stages of regeneration, from initial proliferation to final differentiation. This temporal control is essential, as the signals required to start the growth process are often very different from the signals required to stop it and refine the tissue.
For example, a treatment might begin with a molecule that inhibits the Hippo pathway to stimulate cell division, followed by a second molecule that promotes the formation of blood vessels to nourish the new growth. Finally, a third molecule could be introduced to encourage the cells to mature into the specific types needed for that organ.
The development of these chemical cocktails requires a deep understanding of the cross-talk between different signaling pathways, such as Wnt, Notch, and Hedgehog. By fine-tuning the concentrations and timing of these molecules, researchers can recreate the complex developmental environment of the embryo within the body of an adult patient for restorative purposes.
As our library of regenerative small molecules continues to grow, the possibility of treating complex injuries with a simple injection or topical gel becomes increasingly likely. This would democratize access to advanced regenerative medicine, making it available in standard clinical settings rather than just specialized research hospitals or high-end medical facilities.
Clinical Successes in Fingertip and Bone Growth
The practical application of in situ tissue regeneration has already seen remarkable success in clinical trials, particularly in the regeneration of fingertip bone and nail bed tissue. These areas are unique in humans because they possess a small amount of natural regenerative potential, which researchers have been able to significantly enhance.
By applying a specialized scaffold infused with growth factors and fibrosis inhibitors, surgeons have successfully prompted the body to regrow missing sections of the distal phalanx. This process involves the formation of a blastema-like structure, similar to what is seen in salamanders, which then matures into functional bone, nerve, and skin.
Beyond fingertips, in situ tissue regeneration is being used to heal large bone defects that would otherwise require painful bone grafts or permanent metal implants. By using bone morphogenetic proteins (BMPs) in combination with localized gene therapy, doctors can stimulate the patient's own bone cells to bridge the gap and restore structural integrity.
These successes are not limited to hard tissues; researchers are also making strides in regenerating damaged heart muscle following a myocardial infarction. By injecting small molecules that stimulate the proliferation of existing cardiomyocytes, they have been able to reduce the size of the heart's scar and improve overall cardiac function in animal models.
Each clinical success provides valuable data that helps refine the regenerative pharmacopoeia, moving us closer to the day when we can regrow entire limbs or complex organs. The ability to harness the body's internal resources for healing is proving to be more effective and less prone to rejection than any external technological solution developed.
The Future Paradigm of Restorative Medicine
The shift toward in situ tissue regeneration marks the beginning of a new era in healthcare, moving away from the "replacement medicine" of the 20th century. Instead of relying on mechanical prosthetics or donor transplants—both of which come with significant limitations—we are entering a period of "restorative medicine" where the patient is their own source of healing.
This paradigm shift has profound implications for how we treat chronic diseases, traumatic injuries, and even the natural decline associated with aging. By maintaining the body's regenerative capacity throughout life, we could potentially prevent the organ failure and tissue degeneration that currently characterize the later stages of human existence and medical care.
Moving Beyond Prosthetics and External Transplants
While prosthetics have become incredibly advanced, they still lack the sensory feedback, biological integration, and self-repairing capabilities of natural limbs. In situ tissue regeneration offers the ultimate solution by replacing missing parts with the patient's own living tissue, which is perfectly matched to their unique genetic and physiological profile.
Similarly, organ transplants are currently limited by a chronic shortage of donors and the lifelong need for immunosuppressive drugs to prevent rejection. By growing a new organ in situ, or repairing a damaged one through targeted regenerative therapies, we can eliminate these risks and provide patients with a much higher quality of life and longevity.
The economic impact of this shift is also significant, as the long-term costs of managing chronic organ failure and maintaining prosthetic devices are immense. Regenerative therapies, while potentially expensive to develop, offer a one-time "cure" that restores the patient to full health, reducing the burden on healthcare systems and improving overall economic productivity.
Furthermore, the psychological benefits of restorative medicine cannot be overstated, as patients who undergo in situ tissue regeneration are able to maintain their physical integrity and sense of self. The ability to heal oneself naturally is a powerful motivator and a fundamental shift in the patient-doctor relationship and the healing process.
As we move beyond the era of artificial replacements, the focus of biomedical engineering will increasingly turn toward the creation of bio-instructive materials. These materials will act as temporary guides for the body's own cells, providing the necessary structural and chemical cues to ensure that the regenerated tissue is indistinguishable from the original organ.
Ethical Implications and the Path to Organ Growth
As with any powerful technology, in situ tissue regeneration brings with it a host of ethical considerations that must be carefully navigated by the scientific community. The ability to "reprogram" human cells and activate dormant genes raises questions about the boundaries of biological intervention and the potential for unintended consequences in the genome.
There is also the concern of equity, as these advanced regenerative therapies may initially be available only to those who can afford them, potentially widening the health gap between different socioeconomic groups. Ensuring that the benefits of in situ tissue regeneration are distributed fairly is a major challenge for policymakers and healthcare providers in the future.
The path to full organ growth in situ is also fraught with technical challenges, such as ensuring the correct vascularization and innervation of the new tissue. While we can currently regrow simple structures, the complex architecture of a kidney or a lung requires a level of spatial control that we are only beginning to understand and master.
Despite these challenges, the momentum behind in situ tissue regeneration is unstoppable, driven by the clear clinical need and the rapid pace of biological discovery. As we continue to refine our understanding of the "salamander genes" and the pathways that control them, the dream of total biological restoration is becoming a reality for patients.
Ultimately, the future of medicine lies in our ability to partner with our own biology rather than trying to circumvent it with mechanical or external solutions. By awakening the regenerative potential within us, we can transform the human experience of injury and disease, ushering in an age where the body's capacity to heal is limited only by our understanding.
Also Read
From our network :
- https://www.themagpost.com/post/trump-political-strategy-how-geopolitical-stunts-serve-as-media-diversions
- 10 Physics Numerical Problems with Solutions for IIT JEE
- https://www.themagpost.com/post/analyzing-trump-deportation-numbers-insights-into-the-2026-immigration-crackdown
- EV 2.0: The Solid-State Battery Breakthrough and Global Factory Expansion
- Vite 6/7 'Cold Start' Regression in Massive Module Graphs
- AI-Powered 'Precision Diagnostic' Replaces Standard GRE Score Reports
- Mastering DB2 12.1 Instance Design: A Technical Deep Dive into Modern Database Architecture
- Mastering DB2 LUW v12 Tables: A Comprehensive Technical Guide
- 98% of Global MBA Programs Now Prefer GRE Over GMAT Focus Edition
RESOURCES
- Engineered biomaterials for in situ tissue regeneration | Nature ...
- Biomaterials for In Situ Tissue Regeneration: A Review - PMC
- Engineered biomaterials for in situ tissue regeneration - ADS
- Biomaterials for In Situ Tissue Regeneration: A Review
- Biomaterials for recruiting and activating endogenous stem cells in ...
- Homing of endogenous stem/progenitor cells for in situ tissue ...
- Microneedles for in situ tissue regeneration - ScienceDirect
- Portable hand-held bioprinters promote in situ tissue regeneration
- Oxygen-supplying syringe to create hyperoxia-inducible hydrogels ...
- Biomaterials for in situ tissue regeneration: development and ...
- Distinct Effects of Heparin and Interleukin‐4 Functionalization on ...
- Living joint prosthesis with in-situ tissue engineering for real-time ...
- Long-Term Results of Cell-Free Biodegradable Scaffolds for In Situ ...
- Hyperspectral Tracking of In Situ Tissue Regeneration and ...
- Portable hand‐held bioprinters promote in situ tissue regeneration ...




2 Comments